When you stop breathing repeatedly throughout the night, your body experiences far more than just disrupted sleep. Recent studies from Singapore General Hospital's Sleep Centre reveal that approximately 15% of Singapore's population suffers from obstructive sleep apnea (OSA)—significantly higher than the 1-5% prevalence observed in Western populations.
What makes this particularly concerning? The condition silently damages your cardiovascular system, disrupts metabolic function, and affects brain health every single night you remain untreated. Research published by the National Heart Centre Singapore demonstrates that patients with severe sleep apnea face dramatically elevated risks for life-threatening conditions.
Singapore's unique demographics—with higher prevalence among Chinese, Malay, and Indian ethnic groups due to craniofacial anatomy differences—creates specific health challenges. This guide examines the medical evidence connecting sleep apnea to serious health complications, helping you understand the importance of early diagnosis and appropriate treatment.
How Sleep Apnea Damages Body Systems
What Happens During Each Breathing Pause
Imagine your oxygen levels dropping suddenly while you sleep, triggering an emergency response from your nervous system. This scenario repeats 10, 20, or even 30 times every hour in people with moderate to severe sleep apnea.
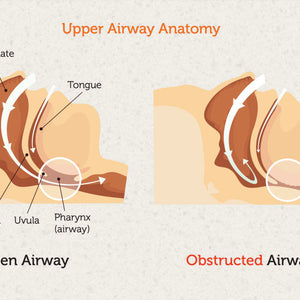
Each airway collapse causes blood oxygen saturation to drop—sometimes below 80% compared to normal levels of 95-100%. Your brain detects this danger and releases stress hormones including adrenaline and cortisol to partially wake you and reopen the airway. This creates sudden spikes in heart rate and blood pressure.
According to cardiovascular research published in the American Heart Association journal, these repeated oxygen drops and pressure surges cause systemic inflammation, damage blood vessel linings, and disrupt normal hormone production. The nightly assault creates permanent structural changes over time.
Why Singapore's Population Faces Elevated Risks
Medical documentation from Singapore General Hospital shows that Asian populations develop sleep apnea at lower body weights compared to Caucasian populations. You might have significant sleep apnea with a BMI as low as 23-25—far below Western thresholds.
The reason? Craniofacial anatomy. Narrower airways, smaller jaw structures, and different fat distribution patterns common among Singapore's ethnic communities increase anatomical vulnerability. Combined with modern lifestyle factors—high-stress work environments, extended sitting hours, and readily available high-calorie foods—these genetic predispositions amplify health risks considerably.
The Heart Connection: Cardiovascular Risks
Blood Pressure and Hypertension
Does your blood pressure remain high despite medications? Sleep apnea frequently explains resistant hypertension. Medical studies document that 50-90% of people with obstructive sleep apnea develop elevated blood pressure from repeated pressure surges during breathing pauses.
Your cardiovascular system never experiences normal nighttime recovery. Instead of the healthy blood pressure dip during sleep that allows healing, you endure constant sympathetic nervous system activation. This sustained elevation damages blood vessel walls, increases heart workload, and accelerates cardiovascular disease progression.
Coronary Artery Disease and Heart Attacks
Groundbreaking research conducted at Singapore General Hospital and National Heart Centre Singapore revealed that nearly half of patients with severe sleep apnea showed atherosclerosis evidence, with 8.7% having calcium scores above 400—indicating 25 times higher heart attack risk than normal.
Oxygen deprivation during apnea episodes causes direct blood vessel wall damage. This triggers lipid and calcium deposits in arterial walls, progressively narrowing and hardening arteries supplying your heart muscle.
International research published in the European Heart Journal demonstrated that patients with obstructive sleep apnea who received coronary stents faced 57% higher risk of major cardiac events. The study followed 1,311 patients across five countries, confirming that OSA independently predicts heart attacks, strokes, and cardiovascular deaths.
Heart Failure and Structural Changes
Medical evidence documents that sleep apnea increases heart failure risk by 140%. Your heart pumps against higher resistance while receiving less oxygen—causing structural chamber changes over time.
The left ventricle enlarges and thickens from increased workload. This remodeling reduces efficiency, pumping less blood with each beat. As function deteriorates, fluid accumulates in lungs and body tissues.
Atrial Fibrillation and Irregular Rhythms
Sleep apnea dramatically increases risk of developing atrial fibrillation, the most common irregular heart rhythm. Singapore research shows structural heart changes from oxygen deprivation disrupting electrical conduction.
People with sleep apnea experience 2-4 times higher AFib rates. The irregular heartbeat causes blood pooling in chambers, forming clots that can travel to the brain causing strokes.
Stroke: A Clear and Present Danger
Research published in Stroke journal found severe obstructive sleep apnea increases stroke risk by 152% in elderly populations. Even after adjusting for hypertension and diabetes, severe sleep apnea independently predicted ischemic stroke.
Comprehensive review in BMC Neurology explains multiple contributing mechanisms:
-
Blood pressure surges rupturing weakened brain vessels
-
Inflammation promoting clot formation
-
Atrial fibrillation creating additional risks
-
Direct vascular damage from oxygen deprivation
National University Heart Centre research found 52% of heart attack patients tested positive for sleep apnea, with 42% having obstructive sleep apnea—underscoring why Singapore cardiologists now routinely screen cardiac patients.
Metabolic Disruption: Diabetes Connection
The Diabetes Relationship
Research in the Singapore Medical Journal reveals bidirectional relationships between sleep apnea and type 2 diabetes. Studies show 50-80% of type 2 diabetics have undiagnosed sleep apnea, while people with moderate to severe OSA face 2.5 times higher diabetes risk.
Intermittent oxygen deprivation triggers stress hormone release—cortisol and adrenaline—signaling your liver to release stored glucose while reducing cellular insulin sensitivity. This creates insulin resistance independent of body weight.
Recent Singapore population studies found women sleeping six hours or fewer nightly had 32% higher type 2 diabetes risk. Combined with sleep apnea, these risks compound substantially.
Oxygen desaturation severity during sleep correlates directly with insulin resistance degree. Studies in Nature Scientific Reports demonstrate that treating sleep apnea improves blood sugar control, with A1C reductions of 0.5-1.0% in patients using therapy consistently.
Metabolic Syndrome
Sleep apnea functions as both consequence and cause of metabolic syndrome—the dangerous clustering of abdominal obesity, high blood pressure, elevated blood sugar, and abnormal cholesterol levels.
Sleep fragmentation disrupts hormones regulating appetite and metabolism. Leptin (the fullness hormone) becomes elevated but ineffective, while ghrelin (hunger hormone) increases. This drives increased caloric intake and cravings for high-calorie, high-carbohydrate foods.
Singapore's high metabolic syndrome prevalence, particularly among middle-aged adults, correlates with undiagnosed sleep apnea rates. Addressing both conditions simultaneously proves essential for successful management.
Body Weight Considerations
The relationship between sleep apnea and weight creates complex challenges. Excess weight increases airway collapse risk, while sleep apnea complicates weight management through hormonal disruption and reduced energy.
However, weight loss alone doesn't always resolve sleep apnea, particularly in Singapore's population where anatomical factors play larger roles than obesity. Many patients with normal BMI still require treatment due to craniofacial structure. Effective management typically requires appropriate therapy combined with comprehensive lifestyle modifications.
Brain Health: Cognitive Decline and Memory Loss
Memory Problems and Brain Structure Changes
University of California, Irvine neurobiologists discovered that obstructive sleep apnea during REM sleep—when most memory consolidation occurs—links directly to early signs of brain changes associated with cognitive decline.
Repeated oxygen deprivation damages brain cells, particularly in memory formation regions. The hippocampus shows measurable shrinkage in people with untreated sleep apnea.
Brain imaging studies reveal reduced gray matter volume in multiple brain regions and white matter changes indicating accelerated brain aging. Cumulative effects of thousands of oxygen drops create permanent structural changes impairing cognitive function.
Can Brain Damage Be Reversed?
Encouraging research from the American Academy of Sleep Medicine indicates brain damage caused by severe sleep apnea may be reversible with treatment. Participants using CPAP therapy showed improvements in damaged structures, with many experiencing almost complete reversal of white matter abnormalities.
While existing structural damage cannot be fully reversed, appropriate treatment halts progression and allows some functional recovery. Patients consistently report better focus, improved productivity, and enhanced quality of life within weeks to months of starting treatment.
Attention, Concentration and Safety Risks
Beyond memory, sleep apnea impairs executive functions including planning, decision-making, problem-solving, and judgment. The prefrontal cortex proves particularly vulnerable to oxygen deprivation and sleep fragmentation.
Singaporeans with untreated sleep apnea often struggle with work productivity, making errors and having difficulty managing complex projects. Students may experience declining academic performance despite adequate study time.
Attention deficits and slowed reaction times create serious safety risks. Research documents motor vehicle accident rates 2-3 times higher among people with untreated sleep apnea. Appropriate treatment dramatically improves attention, concentration, and reaction times.
Depression and Mood Changes
Depression and anxiety occur significantly more frequently in people with sleep apnea. Biological mechanisms include disrupted neurotransmitter function, elevated stress hormones, and inflammation affecting brain chemistry.
Studies indicate 50-60% of people with sleep apnea experience depression symptoms. Many Singaporeans treated for depression without success may have undiagnosed sleep apnea as underlying cause.
Combined medical and therapy approaches prove more effective than single interventions. Some patients experience complete depression symptom resolution after months of effective treatment.
Additional Health Complications
Liver Function
Sleep apnea significantly increases non-alcoholic fatty liver disease (NAFLD) risk and progression to cirrhosis. Intermittent oxygen deprivation causes oxidative stress and inflammation in liver cells, while metabolic dysfunction promotes fat accumulation.
People with moderate to severe sleep apnea show 2-3 times higher rates of abnormal liver enzyme levels. Singapore's high NAFLD prevalence likely reflects undiagnosed sleep apnea contributing to disease progression.
Kidney Disease
Research links sleep apnea to accelerated chronic kidney disease progression through hypertension damage to kidney vessels, disrupted fluid balance, and inflammation affecting tissue. Patients show faster decline in kidney filtration rates.
For Singaporeans with existing kidney disease or diabetes affecting function, treating sleep apnea may slow progression and preserve function longer.
Eye Problems
Sleep apnea associates with several eye conditions including glaucoma, optic neuropathy, and retinal vein occlusion. Blood pressure and oxygen fluctuations may damage delicate blood vessels and nerves.
Studies show 2-10 times higher glaucoma rates among sleep apnea patients. Routine eye examinations help detect complications early when treatment prevents vision loss.
Sexual Function
Men with sleep apnea experience erectile dysfunction rates of 40-70%. Mechanisms include reduced testosterone from disrupted sleep, impaired blood flow from vascular dysfunction, and reduced energy from chronic fatigue.
Sleep fragmentation disrupts normal hormone production rhythms. Testosterone typically peaks during REM sleep, but sleep apnea reduces REM time and disrupts production.
Treatment Approaches and Health Protection
Understanding CPAP Therapy
Continuous Positive Airway Pressure (CPAP) remains the gold standard treatment for obstructive sleep apnea. The therapy delivers pressurized air through a mask, keeping your airway open throughout the night.
Multiple clinical studies demonstrate CPAP therapy significantly reduces cardiovascular risks when used consistently. Blood pressure typically decreases by 5-15 mmHg within weeks. Heart muscle function improves as the organ experiences less nighttime stress.
For maximum benefit, CPAP requires consistent use for at least 4-6 hours nightly. Studies show patients using therapy 6+ hours nightly experience the greatest risk reductions.
Available CPAP Equipment Options
Singapore patients have access to various CPAP technologies suited to different needs:
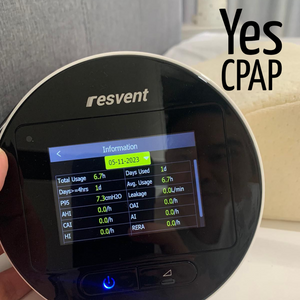
Auto-Adjusting CPAP Machines: These devices monitor breathing patterns and automatically adjust pressure delivery throughout the night. Models like the Resvent iBreeze Auto CPAP provide sophisticated algorithms responding to changing requirements during different sleep stages.
Portable Travel Options: For those who travel frequently or enjoy camping, compact devices like the Resvent iBreeze Plus with battery capability maintain therapy effectiveness in portable form.
BiPAP Devices: For patients requiring different pressures during inhalation and exhalation, BiPAP machines provide more comfortable breathing patterns for complex cases.
Mask Selection: Proper mask fit proves crucial for therapy success. Options include nasal pillows, nasal masks, and full-face designs like the Philips Dreamwisp. Finding the right fit requires professional guidance and often trying multiple styles.
Metabolic Improvements
Appropriate therapy improves insulin sensitivity and blood sugar control in diabetic patients. A1C levels often decrease by 0.5-1.0% with consistent use. Some pre-diabetic patients avoid diabetes progression through treatment combined with lifestyle modifications.
Restoration of normal sleep architecture allows proper hormone regulation. Leptin and ghrelin levels normalize, reducing excessive appetite. However, treatment alone rarely causes significant changes without accompanying dietary and exercise modifications.
Monitoring Treatment Effectiveness
Modern CPAP machines track detailed usage data including hours per night, mask leak rates, and residual breathing disruptions. This allows healthcare providers to verify effectiveness and make necessary adjustments.
Regular follow-up ensures optimal therapy, addresses issues affecting compliance, and monitors for changes requiring pressure adjustments.
Who Should Get Tested
High-Risk Groups
Men over 40 with BMI above 23, anyone with neck circumference over 16 inches (men) or 15 inches (women), people with resistant hypertension, and anyone with atrial fibrillation or heart failure should pursue testing.
Those with type 2 diabetes face 50-80% likelihood of having sleep apnea. Stroke survivors should be evaluated as prevalence exceeds 60% in this population.
Recognizing Symptoms
Beyond loud snoring and witnessed breathing pauses, many symptoms are subtle: morning headaches, dry mouth upon awakening, excessive daytime sleepiness, difficulty concentrating, mood changes, and frequent nighttime urination.
If you or your partner notice these symptoms, schedule evaluation promptly.
Screening Tools
The STOP-BANG questionnaire provides simple screening assessing eight risk factors. Scores of 3 or higher indicate moderate to high risk requiring diagnostic testing.
The Epworth Sleepiness Scale measures daytime sleepiness severity, helping distinguish normal fatigue from pathological sleepiness.
Diagnostic Testing
Polysomnography in sleep laboratories remains the diagnostic gold standard. Singapore offers services at Singapore General Hospital Sleep Centre, National University Hospital, and Changi General Hospital.
Home sleep testing provides convenient, cost-effective alternatives for many patients, though laboratory studies offer more comprehensive data.
Prevention Strategies
Weight Management
Achieving healthy body weight represents an important modifiable risk factor. Even modest weight loss of 10-15% can reduce severity in some patients. However, for Singapore's population where anatomical factors play significant roles, weight loss alone may not resolve the condition.
Working with nutritionists familiar with local cuisine helps develop sustainable eating patterns. Reducing late-night eating, choosing healthier hawker center options, and increasing vegetable portions contributes to gradual improvement.
Sleep Position Training
Sleeping on your back worsens sleep apnea as gravity pulls tongue and soft tissues backward. Many people experience reduced apnea when sleeping on sides.
Positional therapy using special pillows or devices preventing back sleeping reduces severity for position-dependent patients. This low-cost intervention helps some patients, though severe cases typically require more comprehensive approaches.
Alcohol and Sedative Avoidance
Alcohol and sedative medications relax throat muscles, increasing airway collapse frequency and severity. Avoiding alcohol 3-4 hours before bedtime reduces severity.
Many over-the-counter and prescription sleep aids worsen sleep apnea. Discuss all medications with your doctor if you have or suspect the condition.
Smoking Cessation
Smoking increases risk through upper airway inflammation, increased fluid retention in tissues, and disrupted sleep architecture. Smokers face 2-3 times higher risk.
Singapore's comprehensive cessation programs through polyclinics provide medications, counseling, and support for quitting.
Regular Exercise
Physical activity improves sleep apnea through multiple pathways including better muscle tone, improved sleep quality, and reduced inflammation. Regular exercise reduces severity even without significant changes in body weight.
Starting with 150 minutes of moderate activity weekly provides substantial health benefits.
Frequently Asked Questions
Can sleep apnea cause heart attacks during sleep?
Yes, sleep apnea significantly increases heart attack risk during sleeping hours. Research documents people with severe untreated sleep apnea face 57% higher risk of major cardiac events. Repeated oxygen drops, blood pressure surges, and stress hormone release create conditions triggering heart attacks, with early morning hours being particularly dangerous when apnea worsens during REM sleep. Appropriate treatment reduces this risk by stabilizing oxygen levels and blood pressure throughout the night.
How does sleep apnea affect diabetes management?
Sleep apnea makes blood sugar control significantly more difficult. Singapore Medical Journal research shows 50-80% of type 2 diabetics have undiagnosed sleep apnea contributing to poor control. Treatment improves insulin sensitivity and typically lowers A1C by 0.5-1.0% within 3-6 months. Many diabetic patients find blood sugar management becomes easier after starting appropriate therapy, with more stable glucose levels throughout day and night. Combined approaches addressing both conditions provide optimal metabolic control.
What blood pressure changes can I expect after starting treatment?
Most patients using therapy consistently experience blood pressure reductions within 2-4 weeks. Clinical evidence shows average decreases of 5-15 mmHg in systolic pressure and 3-10 mmHg in diastolic pressure. Greatest improvements occur in patients with resistant hypertension. Benefits increase with adherence—using therapy 6+ hours nightly provides maximum cardiovascular protection. Some patients reduce or eliminate blood pressure medications under medical supervision after several months, though medication adjustments should only occur under physician guidance.
Does sleep apnea increase stroke risk in younger adults?
Yes, sleep apnea increases stroke risk across all age groups. Research published in Stroke journal demonstrates that having sleep apnea multiplies baseline risk by approximately 60% regardless of age. Younger adults with severe sleep apnea face stroke risks comparable to much older adults without the condition. Singapore studies show 60-70% of stroke patients have undiagnosed sleep apnea. Young adults experiencing strokes without traditional risk factors should undergo evaluation.
Will treating my sleep apnea help with weight management?
Treatment makes weight management easier but rarely causes weight loss without lifestyle modifications. Untreated sleep apnea disrupts hormones regulating appetite and metabolism. Starting appropriate therapy normalizes these hormones within weeks—most patients report reduced appetite, decreased cravings, and increased energy for exercise. However, successful weight management requires combining treatment with proper nutrition and regular physical activity. Studies show patients using therapy successfully lose more weight compared to those with untreated sleep apnea following identical diet and exercise programs.
Can sleep apnea cause permanent brain damage?
Yes, prolonged untreated sleep apnea causes measurable structural brain changes. Brain imaging studies show reduced gray matter volume in memory centers and white matter damage indicating accelerated aging. However, research demonstrates that starting appropriate treatment halts progression and some patients experience almost complete reversal of white matter abnormalities. Memory, attention, and cognitive function improve within weeks to months of starting treatment. Early diagnosis proves critical—longer untreated duration causes more permanent damage.
How quickly will I feel better after starting treatment?
Most patients notice improvements within days to weeks, though maximum benefits require 1-3 months of consistent use. Daytime sleepiness and fatigue often improve dramatically within the first week. Concentration and reaction times begin improving within 2-4 weeks. Research shows blood pressure reductions occur within 2-4 weeks. Cognitive function improvements continue progressing over 2-3 months. Cardiovascular benefits accumulate over months to years. Patients using therapy 6+ hours nightly experience faster and more complete benefits compared to those with inconsistent use.
Should I stop my blood pressure medications if treatment lowers my pressure?
Never adjust blood pressure medications without consulting your doctor. While treatment often reduces blood pressure significantly, medication adjustments require medical supervision. Your physician will monitor blood pressure trends over several weeks to months before making changes. Some patients eventually reduce or eliminate medications after 3-6 months of consistent therapy use, but this must occur under supervision with careful monitoring. Focus on using therapy consistently every night and monitoring blood pressure regularly at home. Share this data with your doctor for appropriate medication management decisions.
Is sleep apnea hereditary in Singapore families?
Yes, sleep apnea has strong hereditary components affecting Singapore families across all ethnic groups. Genetic factors influencing jaw size and shape, airway dimensions, tongue size, and fat distribution all contribute to risk. Research indicates family members of sleep apnea patients face 2-4 times higher risk. This proves particularly significant in Asian populations where anatomical factors play larger roles. Children of parents with sleep apnea should undergo evaluation if they snore or show sleep difficulties. Genetic predisposition doesn't guarantee development—lifestyle factors significantly influence whether susceptibility manifests as clinical disease.
What is the connection between sleep apnea and memory loss?
Sleep apnea causes memory problems through multiple mechanisms. UC Irvine research shows repeated oxygen drops directly damage hippocampus neurons essential for forming new memories. Brain imaging shows measurable hippocampus shrinkage. Severely fragmented sleep prevents adequate time in deep sleep stages when memory consolidation occurs. Additionally, disrupted sleep prevents normal clearance of beta-amyloid proteins—proteins accumulating in Alzheimer's disease. Appropriate treatment halts further memory decline and may improve function over 3-6 months, though existing brain damage cannot be reversed. Anyone experiencing unexplained memory problems should undergo evaluation.
Conclusion
Sleep apnea represents a serious systemic disease affecting cardiovascular, metabolic, neurological, and multiple other body systems. Research from Singapore General Hospital and National Heart Centre Singapore documents dramatically elevated risks for heart disease, stroke, diabetes, and cognitive decline demanding urgent attention.
Understanding these serious complications motivates proactive screening and appropriate treatment. The encouraging news? Effective treatment significantly reduces or eliminates many health risks, protecting your heart, brain, and overall wellbeing.
If you experience snoring, breathing pauses, daytime sleepiness, or any conditions strongly associated with sleep apnea—resistant hypertension, atrial fibrillation, type 2 diabetes, or stroke—schedule diagnostic testing promptly. Singapore offers comprehensive services including laboratory sleep studies at major hospitals and convenient home testing options.
Taking action today protects your cardiovascular health, preserves cognitive function, and prevents serious complications that could otherwise develop silently over years of untreated sleep apnea.